Does Snoring Surgery Work?
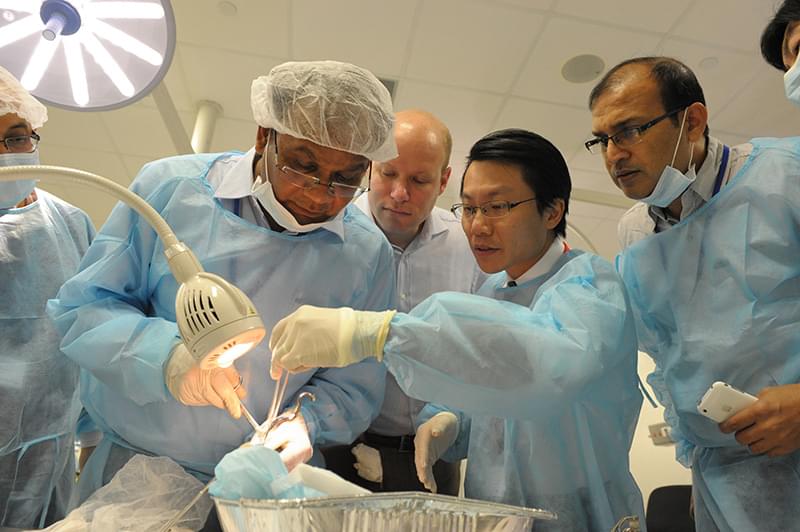
by Dr Kenny Pang
Treatment depends on the type and severity of your sleep apnea.
The severity of a person’s obstructive sleep apnea (OSA) can be classified according to the AHI (apnea-hypopnea index) and lowest oxygen saturation levels (LSAT) recorded during the sleep test. The severity is usually graded as the worst of the two, based on the American Academy of Sleep Medicine (AASM) Guidelines.
| Severity | AHI | LSAT |
|---|---|---|
| Mild OSA | 5 - 14 | 86% - 95% |
| Moderate OSA | 15 - 29 | 75% - 85% |
| Servere OSA | > 30 | < 75% |
In general, patients with snoring / obstructive sleep apnea are classified as those with a “global” problem, that is, obesity compounded with a “local” anatomical problem (huge tonsils, long thick palate, big tongue or a small jaw).
Patients with a "global" problem are advised to:
- Follow a strict trial of weight loss
- Exercise adequately and regularly
- Consult a dietitian / nutritionist for dietary advice
- Regularly follow up on the treatment of their condition
- Wear a nasal mask for continuous positive airway pressure (CPAP) every night during sleep as a trial (even if the patient is considering surgery, as CPAP is reversible and non-invasive).
Surgery may be recommended to correct the condition of patients with huge tonsils, huge adenoids, thick redundant palate and/or a huge tongue. Correcting nasal and palate problems together will significantly improve sleep apnea eradication success rates. About 70% of patients with sleep apnea suffer from airway obstruction because of their palates.
Upper airway surgery is for selected OSA patients who are deemed (by the sleep specialist) to have good prognosis after surgery. This upper airway surgery may include the nose and/or palate with or without the tongue reduction.
Very obese patients with a body mass index (BMI) above 40 are also advised to consult a bariatric (laparoscopic gastric/stomach banding) surgeon. Occasionally, weight reduction medication is considered for patients who are unable to modify their lifestyle for a period of six months. Throughout this period, CPAP must also be strictly adhered to.
Patients with morbid obesity and/or severe diseases like congestive heart failure, and/or respiratory/lung failure may be offered the option of a tracheostomy (surgery performed to create an artificial hole in the airway in the neck).
In obstructive sleep apnea, collapse of the upper airway is usually multi-level.
How snoring and sleep apnea (apnoea) are treated depends on the type and severity of the condition.
Obstructive sleep apnea (OSA) has been known since the 1960s. Management of obstructive sleep apnea has evolved since, and CPAP alone is no longer deemed the gold standard for every patient — CPAP therapy has huge limitations and shortcomings, especially in terms of patient compliance.
In a large-scale study that I co-authored, we found that the compliance rate of CPAP over the last 20 years is only 35% to 40% at best (Rotenberg et al., 2016). Despite the advances in technology and the many upgrades in the CPAP machine, the compliance (usage) rate of patients are persistently at best 35% to 40% overall.
Long-term studies have shown that in over 20,000 patients studied, after seven years of either CPAP or Uvulopalatopharyngoplasty (UPPP) surgery, mortality in CPAP patients was twice as high as that of surgery patients (Weaver et al., 2004).
A landmark scientific paper published in the New England Journal of Medicine (2016), showed that in over 2600 patients, after an 8 year period, patients who used CPAP had the same risk of heart failure, heart attacks, strokes and chest pains, as patients who did not use CPAP.
Obstructive sleep apnea (OSA) surgery has also been found to reduce the incidence of cardiovascular complications such as heart failure, heart attacks, and strokes in OSA patients (Lee et al., 2018).
In obstructive sleep apnea (OSA), collapse of the upper airway is usually multi-level — at the level of the nose, palate, base of tongue, and/or the lateral pharyngeal walls.
Let’s take a closer look at the different anatomy that can cause airway obstruction.
Nose
Nose surgery is important because:
- The nose represents 50% of the airway (the other 50% is the mouth), hence, having a clear nasal passage is fundamental.
- It is well known that the nose represents up to 60-70% of the entire upper airway, and its importance is in being open and allowing the patient to breathe.
- A clear nose is important for a patient who is using the CPAP machine, as it helps in the latter’s usage and improves patient compliance.
- Nose surgery also helps reduce snoring and obstructive sleep apnea (OSA) to a good extent.
Note: Nose surgery aline is at best 20% to 30% effective in treating obstructive sleep apnea (OSA). It should be done with other procedures, like palate or tongue surgery, if the patient has moderate or severe obstructive sleep apnea.
Palate
Palate surgery is important because:
- 70% to 80% of snoring arise from palate problems.
- Surgery to the palate will reduce snoring and obstructive sleep apnea (OSA) effectively.
- The correct type of palate surgery is important to prevent complications.
- Palate reconstruction is now the best method of surgery to correct palate-related issues.
- The recently (2007) invented Pang's Expansion Sphincter Pharyngoplasty (PESP) technique (invented by Pang KP) has been shown to be over 80% effective in helping selected patients with obstructive sleep apnea (OSA).
Tongue
Tongue surgery is important because:
- The tongue may contribute to sleep apnea during an obstruction.
- The tongue contains fat tissue as well (a sizeable amount in fact).
- The tongue needs to be treated if the tongue is causing an obstruction.
- The tongue may be the cause of airway obstruction in around 30% of patients with sleep apnea.
For optimal surgical success rate, the correct procedure needs to be selected for the correct patient; not every patient should have surgery, and surgery can be very successful for a selected group of OSA patients.
